RevBrasAnestesiol.2017;67(5):468---471
REVISTA
BRASILEIRA
DE
ANESTESIOLOGIA
PublicaçãoOficialdaSociedadeBrasileiradeAnestesiologiawww.sba.com.br
SCIENTIFIC
ARTICLE
A
comparison
of
three
different
needles
used
for
spinal
anesthesia
in
terms
of
squamous
epithelial
cell
transport
risk
夽
Ünal
Kantekin
C
¸i˘
gdem
a,∗,
¸ahin
S
Sevinc
¸
b,
Bolat
Esef
c,
Öztürk
Süreyya
a,
Gencer
Muzaffer
a,
Demirel
Akif
aaBozokUniversity,SchoolofMedicine,DepartmentofAnesthesiology,Yozgat,Turkey bBozokUniversity,SchoolofMedicine,DepartmentofPathology,Yozgat,Turkey cFıratUniversity,SchoolofMedicine,DepartmentofAnesthesiology,Elazı˘g,Turkey
Received23January2016;accepted20July2016
Availableonline12August2016
KEYWORDS
Spinalanesthesia; Cerebrospinalfluid; Spinalneedles; Epithelialcells
Abstract
Backgroundandobjectives: Toinvestigatethedifferencesinthenumberofsquamousepithelial cellscarriedtothespinalcanalbythreedifferenttypesofspinalneedletipofthesamesize. Methods:Patientswereallocatedintothreegroups(GroupI,GroupII,GroupIII).Spinal anes-thesiawasadministeredtoGroupI(n=50)usinga25GQuinckeneedle,toGroupII(n=50)using a25Gpencilpointspinalneedle,andtoGroupIII(n=50)usinganon-cuttingatraumaticneedle withspecialbending.Thefirstandthirddropsofcerebralspinalfluid(CSF)samplesweretaken fromeachpatientandeachdropwasplacedonaslideforcytologicalexamination.Nucleated andnon-nucleatedsquamousepithelialcellsonthesmearpreparationswerecounted. Results:There wasstatistically significantdifference between thegroups inrespect tothe numberofsquamousepithelialcellsinthefirstdrop(p<0.05).GroupIIIhadlowernumberof squamousepithelialcellsinthefirstdropcomparedtothatofGroupIandGroupII.Meanwhile GroupIhadhighernumberofsquamousepithelialcellsinthethirddropcomparedtotheother groups.Thenumberofsquamousepithelialcellsinthefirst andthirddropswasstatistically similarineachgrouprespectively(p>0.05foreachgroup).
Conclusions:Inthisstudyofdifferentneedletips,itwasseenthatwithatraumaticneedlewith specialbendingasignificantlysmallernumberofcellsweretransportedwhencomparedtothe Quincketipneedles,andwithpencilpointneedles.
©2016SociedadeBrasileiradeAnestesiologia.PublishedbyElsevierEditoraLtda.Thisisan openaccessarticleundertheCCBY-NC-NDlicense( http://creativecommons.org/licenses/by-nc-nd/4.0/).
夽
Presentationatameeting:TurkishSocietyofAnaesthesiologyandReanimation,49thNationalCongress,2---6December2015,Antalya, Turkey.
∗Correspondingauthor.
E-mail:drcgdm@hotmail.com(Ü.K.C¸i˘gdem).
http://dx.doi.org/10.1016/j.bjane.2016.07.011
Comparisonofthreedifferentneedlesusedforspinalanesthesia 469
PALAVRAS-CHAVE
Raquianestesia; Líquido
cefalorraquidiano; Agulhasespinhais; Célulasepiteliais
Comparac¸ãodetrêsagulhasdiferentesusadaspararaquianestesiaemrelac¸ão aoriscodetransportedecélulasepiteliaisescamosas
Resumo
Justificativaeobjetivo: Investigar as diferenc¸as no número decélulas epiteliais escamosas transportadaspara ocanal medularportrêstiposdiferentes depontasdeagulhasespinhais domesmotamanho.
Métodos: Os pacientes foram alocados em três grupos (Grupo I, Grupo II, Grupo III). RaquianestesiafoiadministradaaospacientesdoGrupoI(n=50)comagulhaQuinckede25G, doGrupoII(n=50)comagulhaespinhalpontadelápisde25GedoGrupoIII(n=50)comagulha atraumáticanãocortantedecurvaturaespecial.Aprimeiraeterceiragotasdelíquido cefalor-raquidiano(LCR)foramcolhidasdecadapacienteparaamostraecadagotafoicolocadaem lâminaparaexamecitológico.Ascélulasepiteliaisescamosasnucleadasenãonucleadassobre aslâminasdeesfregac¸oforamcontadas.
Resultados: Houve diferenc¸a estatisticamente significativa entre os grupos em relac¸ão ao númerodecélulasepiteliaisescamosasnaprimeiragota(p<0,05).OGrupoIIIapresentouum númeromenordecélulasepiteliaisescamosasnaprimeiragota,emcomparac¸ãocomosgrupos IeII,enquantooGrupoIapresentouumnúmeromaiordecélulasepiteliaisescamosasna ter-ceiragota,emcomparac¸ãocomosoutrosgrupos.Osnúmerosdecélulasepiteliaisescamosasna primeiraeterceiragotasforamestatisticamentesemelhantesemcadagrupo,respectivamente (p>0,05,paracadagrupo).
Conclusões: Neste estudo de pontas de agulha diferentes, verificamos que com a agulha atraumática decurvaturaespecial onúmerode célulastransportadas foisignificativamente menor,emcomparac¸ãocomasagulhasQuinckeepontadelápis.
©2016SociedadeBrasileiradeAnestesiologia.PublicadoporElsevierEditoraLtda.Este ´eum artigo OpenAccess sobumalicenc¸aCCBY-NC-ND( http://creativecommons.org/licenses/by-nc-nd/4.0/).
Introduction
During spinal anesthesia, the tip of the needle acts as a
bistouryand causesepidermal fragmentstobe implanted
into the spinal canal.1 Epidermoid tumors are extremely
raretumorsofthecentralnervoussystem.2Intraspinal
epi-dermoid tumors are known to develop as a result of the
transportofepidermalsquamousepithelialcellsbytrauma,
spinalanesthesia,surgeryandlumbarpuncture.3---5Previous
studieshaveshownthattheuseofsmallerdiameterneedles
andallowingafewdropsofCSFflowduringlumbarpuncture
reducesthenumberoftransportedcells.6
Inthisstudy,throughcytologicalexaminationofthefirst
andthirddropsofcerebrospinalfluidcollectedduringspinal
anesthesia,itwasinvestigatediftherewereanydifferences
in thenumber of squamousepithelial cells carriedto the
spinal canal by spinal needles of the same size but with
threedifferenttiptypes (25Gatraumatic, 25Gpenciltip,
25GQuincke).
Methods
Following the approval of the Ethics Committee, 150
patients undergoing surgery usingspinal anesthesia, aged
between18and65 years,ASA I-IIweredividedintothree
groupsof50(GroupI,GroupII,GroupIII).Thestudyincluded
onlythesubjectswhosefirstpuncturewassuccessful.
Spinalanesthesiawasadministeredusinga25GQuincke
needletothe50patientsinGroupI,usinga25Gpencilpoint
spinalneedletothe50patientsinGroupIIandusinga
(non-cutting)atraumatic needlewithspecialbendingtothe50
patientsinGroupIII.
Writteninformedconsentwasobtainedfromallpatients.
Aftertakingthepatientstotheoperatingroom,Intravenous
(IV) access was established and heart rate, non-invasive
arterial blood pressure, and peripheral oxygen saturation
(SpO2)weremonitoredroutinely.
Sedation was administered as Intravenous (IV)
0.05mg.kg−1 midazolam. With the patient in a seated
position,thespinalneedlewasinsertedthroughtheL4-5or
L5-S1interspaceandthearrivalofcerebrospinalfluidwas
observed. 0.5% hyperbaric bupivacaine wasadministered.
Inallthe groups,the firstandthird dropsofCSFsamples
weretakenandeachdropwasplacedontoaseparateslide.
TheCSFsamplesweresmearedtothesurfaceoftheslide
bytouchinganotherslidetothefirstslide.Asaresult,two
slideswere preparedfor each dropfor cytological
exami-nation.The slideswerestainedwithhematoxylin&eosinin
theMedicalPathologyLaboratoryandevaluatedunderlight
microscope by a pathologist blinded tothe study groups.
Thetotalnumberofnucleatedandnon-nucleatedsquamous
epithelialcells derived fromthelayersof epidermiswere
countedonthewholesurfaceofthetwoslidesofeachdrop
andrecorded.
DataanalysiswasperformedusingSPSS 21.0statistical
softwarepackage.Thecomplianceofdatawithnormal
dis-tributionwasevaluatedwiththeKolmogorov---Smirnovtest.
TheKruskal---Wallistestwasusedforcomparisonsbetween
470 Ü.K.C¸i˘gdemetal.
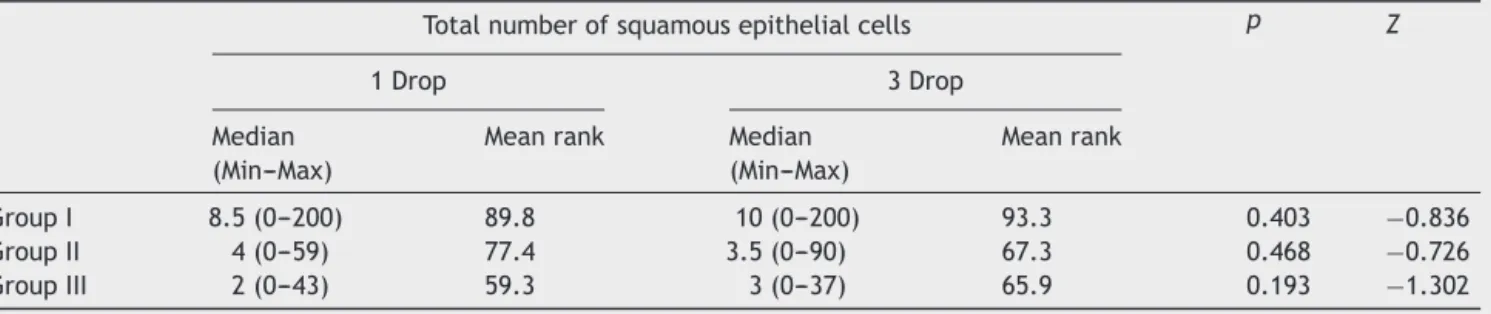
Table1 ComparisonofthetotalnumberofsquamousepithelialcellsdetectedinwholesurfaceoftwoslidesofCSFingroups fordrop1and3(mean±SD).
Totalnumberofsquamousepithelialcells p Z
1Drop 3Drop
Median (Min---Max)
Meanrank Median (Min---Max)
Meanrank
GroupI 8.5(0---200) 89.8 10(0---200) 93.3 0.403 −0.836
GroupII 4(0---59) 77.4 3.5(0---90) 67.3 0.468 −0.726
GroupIII 2(0---43) 59.3 3(0---37) 65.9 0.193 −1.302
originated,theTukeyHSDtestwasapplied.Thevalueswith probabilitylowerthan(p)˛=0.05wereassumedtobe
sig-nificant.
Results
Thepatientscomprised51.2%femalesand48.8%maleswith ameanageof45.53±17.20years.
A statistically significant difference was determined betweenthegroups inthenumber ofsquamousepithelial cellsinthefirstdrop(p<0.05).WhencomparedtoGroupI andGroupII,thevaluesofGroupIIIwerelower.
A statistically significant difference was determined betweenthegroups inthenumber ofsquamousepithelial cellsin thethird drop.The valuesof GroupIwerehigher thanthoseofGroupsIIandIII.
Nostatisticallysignificantdifferencewasdeterminedin any of the groups between the first and third drops, in termsofthenumberofsquamousepithelialcells(p>0.05) (Table1).
Discussion
Sincethetimeoffirstmanufacturein1891,theneedlesused
inspinalanesthesiahavebeenproducedindifferenttypes.
Withthedevelopmentoftechnology,needlesarenow
man-ufacturedwithdifferenttipsanddiameters.Spinalneedles
in current use have different structures such asQuincke,
Whitacre,Sprotte,Atraucan(atraumatictip)andSpinoject.
ApencilpointspinalneedleissimilartotheWhitacreand
Sprottetypespinalneedlesandisavailableinvarioussizes
such as 22, 25 and 27G. Although the diversity in spinal
needles has essentially been made with the intention of
reducingpost-spinalheadache,needletipsarealso
impor-tantwithregardtothenumberofcellstransportedintothe
spinalcanalduringspinalanesthesiaapplication.
Intraspinal epidermoid tumors are quite rare tumors
thatconstituteonly1% ofspinaltumorsinall agegroups.
Iatrogeniclumbarintraspinalepidermoidtumorswerefirst
identifiedin1950afterrecurrentantibioticinjectionstothe
subarachnoidspace.7
Squamous epithelial cells from which the tumor
origi-nates can be implanted into the subarachnoid space by
trauma,spinalanesthesia,surgeryandlumbarpuncture.4---6
In has been stated in a previous study that the rate
of most cell implantation into the spinal canal is 33.3%
throughepidural needles.8 Manno et al. reported that in
41%ofcases,intraspinalsquamouscelltumorsarecausedby
thecellsimplantedintotheintraspinalcanalduringlumbar
puncture.9
In another study,it was stated that the rate of tissue
transportbyspinalneedlesisaround75%butinCSF,no
tis-sue couldbeshown.6 Inanotherstudy of4 cadavers,27G
Quincke,Sprotte,andWhitacreneedleswerecomparedand
itwasshownthatinCSF,ahigherrateofbenignsquamous
epithelialcellsweretransferredbyQuincketypeneedles.10
In the current study, evaluation was made of the
cere-brospinal fluid of a total of 150 patients to whom spinal
anesthesiawasadministeredwith25GQuincke,atraumatic,
and pencil point needles. The results showed that in the
groupwhereQuincketipneedleswereused,thesquamous
epithelialcellcountwassignificantlyhigher.
InastudybyTaveiraetal.,using25GQuincketipspinal
needles,itwasshownthatof39patients,squamous
epithe-lialcellswerefoundintheCSFof35patients.2Inthecurrent
study,squamousepithelialcellswerepresentinboththe1st
and3rddropsinall3groups.However,althoughtheneedle
tipswereofthesamesize,inthegroupwhereatraumatic
needles wereused,thenumberof cells weresignificantly
lowerwhencomparedtotheothertwogroups.Inthe
cur-rent study,while thenumber of cells in the group where
Quincke needles wereusediscompatiblewiththe results
ofTaveiraetal.,itisveryhighcomparedtotheatraumatic
needlegroup.
Previousstudiesinliteraturehaveindicatedthat
allow-ingafewdropsofCSFflowwith25GQuinckeandWhitacre
needlesprovideswashingoftissuefragments.6However,in
theTaveiraetal.studywhichevaluatedthenumberofcells
inthe1stand3rddrops,nodifferencewasfoundbetween
thedrops.Anotherpublicationhasalsostatedthatallowing
CSFflowofbetween8and12dropsdoesnotreducetherisk
oftransportationofepithelialcells.11 Inthecurrentstudy,
therewasnostatisticallysignificantdifferenceinthe
num-berofcellsbetweenthefirstandthethirddrops,whichwas
consistentwiththefindingsinliterature.
In conclusion, the results of this study using different
needletipsdemonstratedthat withatraumaticneedles, a
significantlysmallernumberofcellsweretransportedwhen
comparedtoQuincketipneedles,andwithpencilpoint
nee-dles,althoughnotstatisticallysignificant,ahighernumber
ofcells werecarriedcomparedtothegroup where
atrau-matictipneedleswereused.Whenselectingtheneedletip
foruseindailypractice,squamouscelltransportrateshould
Comparisonofthreedifferentneedlesusedforspinalanesthesia 471
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.Critchley M, Ferguson FR. The cerebrospinal epidermoids (Cholestealoma).Brain.1928;51:334---84.
2.TaveiraMHC,CarneiroAF,RassiGG,etal.Thereishigh inci-denceofskincellsinthefirstandthirddropsofcerebrospinal fluidinspinalanesthesia.RevBrasAnestesiol.2013;63:193---6.
3.PotgieterS,DiminS,LagaeL,etal.Epidermoidtumors asso-ciatedwithlumbarpuncturesperformedinearlyneonatallife. DevMedChildNeurol.1998;40:266---9.
4.ZivET,McCombGJ,KriegerMD,SkaggsDL.Iatrogenicintraspinal epidermoidtumors:twocasesandareviewoftheliterature. Spine.2004;29:E15---8.
5.McDonalJV,KlumpTE.Intraspinalepidermoidtumorscausedby lumbarpuncture.ArchNeurol.1986;43:936---9.
6.CampbellDC,DouglasMJ,TaylorG.Incidenceoftissuecoring withthe25-GaugeQuinckeand Whitacrespinalneedles.Reg Anesth.1996;21:582---5.
7.ChoremisC,EconomosD,PapadatosC,GargoulasA.Intraspinal epidermoidtumours(cholesteatomas)inpatientstreated for tuberculousmeningitis.Lancet.1956;2:437---9.
8.Tunalı Y, Kaya G, TunalıG, Solako˘glu S, Yenice S, Bahar M. Detection of epithelial cell transferin spinal areasby light microscopyanddetermininganytissuecoringviacellculture duringcombinedspinal-epiduralinterventions.RegAnesthPain Med.2006;31:539---45.
9.MannoNJ,UihleinA,KernohanJW.Intraspinalepidermoids.J Neurosurg.1962;19:754---6.
10.PuolakkaR,AnderssonLC,RosenbergPH.Microscopicanalysis ofthreedifferentspinal needletipsafterexperimental sub-arachnoidpuncture.RegAnesthPainMed.2000;25:163---9.