REVISTA
BRASILEIRA
DE
ANESTESIOLOGIA
PublicaçãoOficialdaSociedadeBrasileiradeAnestesiologiawww.sba.com.br
SCIENTIFIC
ARTICLE
Comparison
of
different
stylets
used
for
intubation
with
the
C-MAC
D-Blade
®
Videolaryngoscope:
a
randomized
controlled
study
Dilek
Ömür
a,∗,
Bas
¸ak
Bayram
b,
¸ule
S
Özbilgin
a,
Volkan
Hancı
a,
Bahar
Kuvaki
aaDokuzEylülUniversity,FacultyofMedicine,DepartmentofAnesthesiologyandReanimation, ˙Izmir,Turkey bDokuzEylülUniversity,FacultyofMedicine,DepartmentofEmergencyMedicine, ˙Izmir,Turkey
Received28September2015;accepted18June2016 Availableonline22July2016
KEYWORDS
C-MACD-Blade®
videolaryngoscopy; Intubation; Stylet; Manikin
Abstract
Objective:The angle ofthe C-MAC D-Blade® videolaryngoscope, which is used for difficult
airwayinterventions,isnotcompatiblewithroutinelyusedendotrachealtubes.
Methods:Aprospectiverandomizedcrossoverstudywasperformedcomparingfiveintubation methodsforusewithstandardizedairways,includingusingdifferentstyletsornostylet:Group HS,hockey-stickstylet;GroupDS,D-bladetypestylet;GroupCS,CoPilot® videolaryngoscope rigidstylet®;GroupGEB,gumelasticbougie;andGroupNS,nostylet.Amanikinwasusedto simulatedifficultintubationwithaStorzC-MACD-Blade®
videolaryngoscope.Thedurationof eachintubationstagewasevaluated.
Results:Participantsinthisstudy(33anesthesiologyresidentsand20anesthesiologyexperts) completedatotalof265intubations.Thenumberofattemptsmadeusingnostyletwas signif-icantlygreaterthanthosemadefortheothergroups(p<0.05forgroupNS-groupGEB,group NS-groupDS,groupNS-groupCSandgroupNS-groupHS).Thedurationtopassthevocalcords significantlydifferedamongallgroups(p<0.001).Thetotalintubationdurationwasshortest whenusingD-bladestylet,CoPilotstyletandhockeystickstylet.Althoughnodifferencewas observedbetweenstyletgroups,asignificantdifferencewasfoundbetweeneachofthesethree andnostyletandgumelasticbougie(p<0.05andp<0.001,respectively).
Conclusion:UseofthecorrectstyletleadstoamoreefficientuseoftheStorzC-MACD-Blade®. Inourstudy,theuseoftheD-bladestylet,theCoPilotstyletandthehockeystickstylet pro-videdquickerintubation,allowedeasierpassageofthevocalcords,anddecreasedthetotal intubationduration.Toconfirmthefindingsofourstudy,randomizedcontrolledhumanstudies areneeded.
©2016SociedadeBrasileiradeAnestesiologia.PublishedbyElsevierEditoraLtda.Thisisan openaccessarticleundertheCCBY-NC-NDlicense( http://creativecommons.org/licenses/by-nc-nd/4.0/).
∗Correspondingauthor.
E-mail:drdilekomur@gmail.com(D.Ömür). http://dx.doi.org/10.1016/j.bjane.2016.06.001
DifferentstyletswiththeC-MACD-Blade 451
PALAVRAS-CHAVE Videolaringoscópio
C-MACD-Blade®;
Intubac¸ão;
Estilete; Manequim
Comparac¸ãodediferentesestiletesusadosparaintubac¸ãocomovideolaringoscópio
C-MACD-Blade®:umestudorandômicoecontrolado
Resumo
Objetivo: Oângulo do videolaringoscópioC-D-MACBlade®,usado paraintervenc¸ões em via
aéreadifícil,nãoécompatívelcomostubosendotraqueaisrotineiramenteusados.
Métodos: Um estudo prospectivo,randômico e cruzado foi conduzidopara compararcinco métodosdeintubac¸ãoemmodelodeviaaérea,comousodediferentesestiletesemcinco gru-pos:tacodeHockey;D-blade;CoPilotVL®rígido;GumElasticBougieecontrole(semestilete). Um manequim foi utilizadopara simular intubac¸ãodifícil como laringoscópioStorz C-MAC D-Blade®.Foiavaliadaadurac¸ãodecadafasedeintubac¸ão.
Resultados: Osparticipantesdesteestudo(33residentesdeanestesiologiae20especialistas emanestesiologia)concluíram265intubac¸õesnototal.Onúmerodetentativasrealizadassem estilete foisignificativamentemaiorqueodos outrosgrupos (p<0,05paraSE-GEB,SE-DB, SE-CPeSE-HS).Otempoparapassarpelascordasvocaisfoisignificativamentediferenteentre todososgrupos(p<0,001).Otempototaldeintubac¸ãofoimenorcomousodeD-blade,CoPilot VL®
rígidoetacodeHockey.Emboranãotenhahavido diferenc¸aentreD-blade,CoPilotVL®
rígidoetacodeHockey,umadiferenc¸asignificativafoiobservadaentrecadaumdessestrêse osgrupossemestileteeGumElasticBougie(p<0,05ep<0,001,respectivamente).
Conclusão:AescolhadoestiletecertolevaaousomaiseficientedovideolaringoscópioStorz C-MACD-Blade®.Emnossoestudo,ousodoD-blade,CoPilotVL®rígidoetacodeHockey propor-cionouintubac¸ãomaisrápida,facilitouapassagempelascordasvocaisediminuiuotempototal deintubac¸ão.Paraconfirmarosresultadosdenossoestudo,estudoscontroladoserandômicos comhumanossãonecessários.
©2016SociedadeBrasileiradeAnestesiologia.PublicadoporElsevierEditoraLtda.Este ´eum artigo OpenAccess sobumalicenc¸aCCBY-NC-ND( http://creativecommons.org/licenses/by-nc-nd/4.0/).
Introduction
Despiteimprovements in airwayinterventiondevices,
dif-ficultairwaysremainamongthemostsignificant obstacles
inanesthesiaandemergencymedicine.Inthesurgical
envi-ronment,ithasbeenreportedthat5%and1%ofpatientsare
eligibleforgrade3andgrade4laryngoscopy,respectively. In0.43%ofpatients,directlaryngoscopywithintubationis notpossible.1Studies indicate thatthe incidenceof
diffi-cultintubationvariesfrom0.4%to4.7%;thesenumbersare
higherforobstetricanesthesia(5.7%)andinobesepatients (13.3%).2---4 The incidenceof difficult intubation isgreater
in emergency situations. A multicenter study in the USA
foundthatdifficultieswereencounteredin5%of8937
intu-bationsandreportedthatmorethanonemethodwasused.
The same study found that intubation could not be
com-pleted in 0.84% of patients, and surgical airway opening
wasperformed.5Consequently,theauthorsrecommendthe
earlyuseofdevicesdesignedforusewithdifficultairways topreventcomplications.1
Fordifficultairwayinterventions,videolaryngoscopy(VL) isalife-savingandeffectivemethod.6,7TheC-MACD-Blade®
VL is an increasingly popular laryngoscopy device that is
specially designed for use in difficult intubations.To
bet-ter observe the vocal cords, the C-MAC D-Blade® has a
half-moonshapeandisdesignedwithabroaderanglethan
direct laryngoscopy blades.8 Due to the elliptic and
nar-rowingshapeoftheblade,compatibilitywiththeanatomy
oftheoropharynxispossible.Laryngoscopicvisualizationis
obtained usinga cameralocatedonthe 3.5cm tipof the
C-MAC D-Blade® VL.9 Whereas the angle of vision of the
C-MAC® VLMacintoshbladesnos.3and4are72◦ and60◦,
respectively, the C-MAC D-Blade® VL has a greater angle
of vision of 80◦ due tothe embedded opticlens.10 Thus,
the user can obtain a wider view of the interior of the
mouth.
Theanglingofthebladeisnotcompatiblewiththeangles
ofroutinelyusedendotrachealtubes.Although theC-MAC
D-Blade® VLprovidesbetterimaging,itcanbedifficult to
directtheendotrachealtubewithinthemouthforsuccessful
intubation,andthedurationofintubationmaylengthen.7To
resolvethis problem, it maybe necessary touse a stylet
of an appropriate shape within the intubation tube with
theC-MACD-Blade®VL.11,12Indifficultintubationsthatare
not supported withan appropriate stylet, intubation can
be unsuccessful; the number of intubation attempts can
increase,anditmightbenecessarytoreshapethetubeand
reattemptintubation.Thissituationincreasestheduration
ofintubation, can causetrauma tosoft tissue,and
nega-tivelyaffects thehemodynamics of the patient.Although
the current literature emphasizes the superiority of this
deviceinnormalanddifficultintubationscomparedtoother
laryngoscopydevices,the useof this devicewitha stylet
andimportantpractical issues,suchasstyletpreparation,
remaincontroversial.8
The hypotheses of our study are (1) that not using a
stylet for cases involving C-MAC D-Blade® VL will reduce
the success of intubation and (2) that the use of stylets
withaC-MACD-Blade VL(nostylet[NS]andfourdifferent
stylets:hockey-stick stylet[HS], D-bladetypestylet [DS],
rigidstyletforVL[CS] andgumelasticbougie[GEB]);the
effectsofthesestyletsonintubationsuccess,laryngoscopy
images,theneed for extramaneuvers, complicationsand
thedurationofintubationwereassessed.
Material
Studypopulation
The study began once permission was obtained from the
Dokuz Eylül University Medical Faculty (DEUMF) Research
Ethics Committee. Al-Qasmi et al.13 reported success in
90%ofintubationsusingahockey-stick-shapedstylet.The
hypothesesstudied here are(1) that not usingany stylet
willreducethe successof intubationand(2) thattheuse
of a stylet will increase the success rate. To test these
hypothesesin our planned study and obtain a 20%
differ-encebetweenthegroupswithanalphaerrorof5%and80%
power, the number of insertions required for each group
was determined to be at least 48. Assuming a 10% data
loss, 53 insertions were planned for each group.
Conse-quently,53 physicians(experts or specializationstudents)
fromtheDEUMFAnesthesiologyDepartmentwhohad
expe-rienceusingtheStorzC-MACD-Blade®wereincludedinthis
study.
Randomization
The study followed a prospective randomized crossover
design.Forrandomization,fiveclosedenvelopeswere
pre-pared,eachcontainingthenameofamethod.Allenvelopes
wereleftinabasketbesidetheVLdevice,andthephysician
performingthe interventionchosean envelopeat random
andusedthemethodlistedintheenvelope.
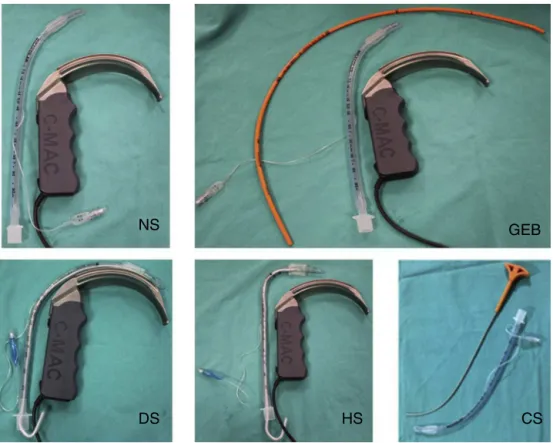
Methodsperformedandpreparation
Thestudycomparedthefollowing5intubationmethodsfor
standardizedairwayvisualization:usingnostyletand4 dif-ferentstylets.Forallintubations,aStorzC-MACD-Blade®
(KarlStorz GmbH& CoKG, Tuttlingen,Germany) external
imagingunitwasusedinthelaryngoscopy.
Forallapplications,anno.7.5standard-cuffintubation
tube was used. In a randomized fashion, all participants
completedtheapplicationsusingnostyletandfourdifferent styletsforintubation.Thestyletmethodsusedinourstudy
wereasfollows:(1)endotrachealintubationwithoutstylet
(nostylet,NS);(2)endotrachealintubationwitha
hockey-stick-shapedstylet(thetipofthestyletwasbenttoforma 90◦angle;hockey-stickstylet,HS);(3)endotracheal
intuba-tionusingtheD-Bladeangle(thetipofthetubewasbentto
forma shapesimilartothe angleof theD-Blade;D-blade
type stylet, DS); (4) endotracheal intubation using a
Co-Pilot®VLrigidstylet(RigidStyletforCo-PilotVL,CS;Magaw
MedicalFortWorth,TX,USA);and(5)intubationusingagum
elasticbougie,whichwaspassedoverthevocalcords;the
tubewasthenslidoverit(gumelasticbougie;GEB)(Fig.1).
Standardizeddifficultairwaysimulation
Difficult intubation conditions were simulated using a
manikin (AirSim® Advance Combo; Trucorp Ltd.; Belfast,
NorthernIreland) forstandardized trauma patient
simula-tionswithremovableteethandadifficultintubationairway.
An appropriatetrauma collar (Ambu® Perfit, Copenhagen,
Denmark)wasusedtopreventmovementof theneckand
chin of the manikin (2). Additionally, to prevent
head-neck movement of the manikin,the manikin wasfixed to
the surgical table with plaster across the forehead and
neck.
Method
Forthestudy,themanikinwasplacedonanoperatingtable.
Following a predetermined order, the randomized
partic-ipants performed each method sequentially. An assistant
waspresenttoaidtheparticipantduringeachendotracheal
intubation attempt. Before each application, the
partici-pant was asked to ventilate the manikin using a Balloon
ValveMask(BVM).The intubationbeganwhenthe
partici-pantfeltready.Foreachprocedure,theparticipantinflated
thecuffofthetube,removedthestyletfromthetube,and
providedventilation fromthe tubetothe BVM.The
assis-tant providedlaryngealexternal interventionifrequested
bytheparticipant.When thesimulatedlungsappearedto
be ventilated, the procedure ended, and intubation was
accepted assuccessful.Incasesrequiring longerthan60s
topass thevocal cords, the attemptwas ended,and the
next attempt began. The manikin was newly ventilated
with the BVM, and all steps were performed again. If 3
attemptswereunsuccessful,theintubationwasassessedas
unsuccessful.
Thestudy teamdeterminedtheintubationsuccess and
the duration of intubation stages. The durations assessed
wereasfollows:(1)durationtovisualizingthevocalcords:
the duration from the moment the participantpicked up
the laryngoscope towhen they observed the vocal cords;
(2)durationtopassthevocalcords:thedurationfromthe
momentthevocalcordswereobservedtowhenthe
intuba-tiontubepassedthevocalcordinterval;(3)durationtocuff
inflation:thedurationfromthemomentthetubepassedthe
vocal cordintervaltowhentheintubation wasperformed
andthecuffwasinflated; (4)durationtofirstventilation: thedurationfromtheinflationofthecufftothefirst
suc-cessful ventilation; and (5) total intubation duration: the
duration from the momentthe participantpicked up the
laryngoscope to when the first successful ventilation was
performed.Thevocalcordimagesontheexternalimaging
unitwereassessedandrecordedbythestudyteam
accord-ingtotheCormakLehaneclassification.14
Achronometer(iPhone5)wasusedtorecordthe
intuba-tiondurations.
Iftheparticipantrequestedextramanipulationtoease
theintubation,thestudyteamrecorded‘‘additional
laryn-gealmanipulation’’(BURP[cricoidpressurewithbackward,
upward, rightward pressure] or OELM [optimal external
laryngeal manipulation]). The upperteeth of themanikin
DifferentstyletswiththeC-MACD-Blade 453
NS
DS
HS
CS
GEB
Figure1 Styletsaccordingtogroup.NS,nostylet;HS,hockey-stickstylet;DS,D-bladetypestylet;GEB,gumelasticbougie;CS, CoPilotVLrigidstylet®.
damaged during the application, this was recorded as a
complicationoftheprocedure.
Correlationofdependentandindependent variablesforstatisticalanalysis
Statisticalanalysiswasperformed usingSPSS15.0for
Win-dows. For the descriptive statistics, categorical variables
are presented as numbers and percentages, and
numer-ical variables are presented as the means and standard
deviations. Numericalvariables betweentwoindependent
groups werecompared usingStudent’st-test for normally
distributeddataandtheMann---WhitneyUtestfordata
with-out normal distribution. Differences between categorical
variablesinindependentgroupsweretestedusingthe
Chi-squareanalysis. To comparethe means of morethan two
groups,aone-wayANOVAtestwasused.Ifdifferenceswere
foundinthevariancehomogeneity,theBonferronitestwas
used.Theresultswereconsideredstatisticallysignificantif p<0.05.
Results
The participantsincluded 33 anesthesiology residentsand
20anesthesiologyexperts(Table1).
Atotal of 265intubationswere completedby the
par-ticipants.Nineteenintubationswerecompletedonthe2nd
attempt, and four were successfully completed on the
3rdattempt.Allintubationswerecompleted withinthree
attempts.Adurationof60sfor thetubetopassthevocal
cords was permitted in the study. A third attempt was
required only for intubationswithout theuse of a stylet.
Whencomparedseparately withtheother groups, no
dif-ferencewasfoundbetweenNSandGEB(p>0.05);however,
Table1 Participantdemographicdata.
n % Mean Min---max
Resident 33 62.3 ---
---Expert 20 37.7 ---
---Age(years) --- 34.7±8.8 25---56
Sex ---
---Female 28 52.8 ---
---Male 25 47.2 ---
Table2 Intubationattempts.
Variable NS HS DS CS GEB n(%)
Numberofattempts
1 40(75.5%) 52(98.1%) 51(96.2%) 52(98.1%) 47(88.7%) 242(92.5%)
2 9(17.0%) 1(1.9) 2(3.8%) 1(1.9) 6(11.3%) 19(7.2%)
3 4(7.5%) --- --- --- --- 4(1.5%)
NS,nostylet;HS,hockey-stickstylet;DS,D-bladetypestylet;GEB,gumelasticbougie;CS,CoPilotVLrigidstylet®.
significantlymoreattempts wererequired for NSthan for
the other groups (p<0.05 for NS-GEB, NS-DS, NS-CS, and
NS-HS).Nosignificantdifferencewasobservedbetweenthe
othergroups interms ofthenumberof attempts(p>0.05
foreachcomparison)(Table2).
Duringallapplications,C/L1---2imageswereobtained.No
statisticallysignificant differencewas found between the
participants’ years of experience and intubation success,
extramanipulationuseandcomplications(p>0.05).
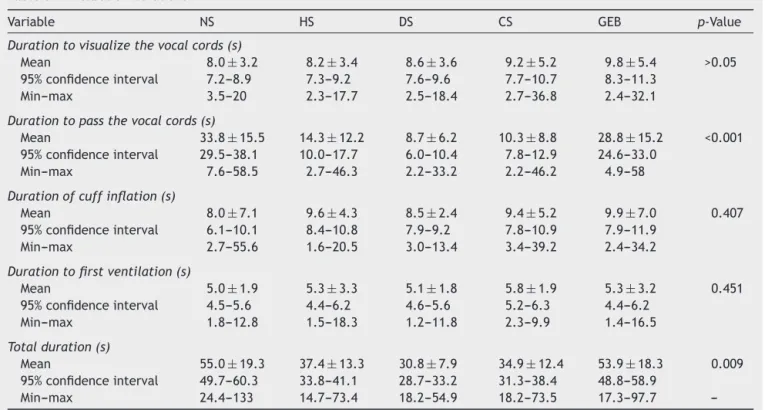
Intubationdurationdid notsignificantlydifferin terms
ofvocalcordvisualizationbetweenthegroups.Durationto
passthevocalcordssignificantlydifferedbetweenallgroups (p<0.001)(Table3).
Durationtopassthevocalcordswasclearlyshorterfor
DS, HS and CS, and no difference were found between
GEBand NS in thisrespect (p<0.05). Asignificant
differ-ence existed between GEB and NS and all other groups
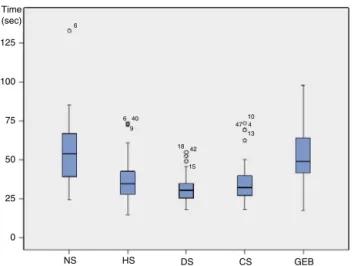
(p<0.001 for all comparisons). No significant difference wasfoundbetweenDS,HSandNS(p>0.05forall compar-isons).Althoughthedurationofcuffinflationappearedtobe shorterintheNSgroup,thedifferencewasnotstatistically significant(p>0.05).Theshortesttotalintubationdurations
wereobtainedusingDS,CSandHS,inthatorder.Although
DS,CSandHSdidnotappeartodiffer,asignificant
differ-encewasfoundbetweeneachofthethreeandNSandGEB
(p<0.05andp<0.001,respectively)(Fig.2).
Intubation without a stylet caused dental damage
complicationsamaximumof15times(28.3%),followedby
GEB with6 incidents (11.3%). When compared separately
withtheothergroups,dentaldamageintheNSgroupwas
significantlygreaterthanthatintheothergroups(p<0.05
for NS-GEB,NS-DS, NS-CS, and NS-HS). No significant
dif-ference wasobservedamongtheother groups interms of
dentaldamage(p>0.05forallcomparisons)(Table4).
Discussion
This study compared intubationswithand without stylets
usingaStorzC-MACD-Blade®onamanikinthatsimulateda
difficultairway;theintubationswereperformedby
anesthe-siologyexpertsandresidents,andtheresultsshowedthat
intubationswithnostyletandwithGEBrequiredlongerto
complete,requiredmoreattemptsandresultedinincreased
Table3 Intubationdurations.
Variable NS HS DS CS GEB p-Value
Durationtovisualizethevocalcords(s)
Mean 8.0±3.2 8.2±3.4 8.6±3.6 9.2±5.2 9.8±5.4 >0.05
95%confidenceinterval 7.2---8.9 7.3---9.2 7.6---9.6 7.7---10.7 8.3---11.3
Min---max 3.5---20 2.3---17.7 2.5---18.4 2.7---36.8 2.4---32.1
Durationtopassthevocalcords(s)
Mean 33.8±15.5 14.3±12.2 8.7±6.2 10.3±8.8 28.8±15.2 <0.001
95%confidenceinterval 29.5---38.1 10.0---17.7 6.0---10.4 7.8---12.9 24.6---33.0
Min---max 7.6---58.5 2.7---46.3 2.2---33.2 2.2---46.2 4.9---58
Durationofcuffinflation(s)
Mean 8.0±7.1 9.6±4.3 8.5±2.4 9.4±5.2 9.9±7.0 0.407
95%confidenceinterval 6.1---10.1 8.4---10.8 7.9---9.2 7.8---10.9 7.9---11.9
Min---max 2.7---55.6 1.6---20.5 3.0---13.4 3.4---39.2 2.4---34.2
Durationtofirstventilation(s)
Mean 5.0±1.9 5.3±3.3 5.1±1.8 5.8±1.9 5.3±3.2 0.451
95%confidenceinterval 4.5---5.6 4.4---6.2 4.6---5.6 5.2---6.3 4.4---6.2
Min---max 1.8---12.8 1.5---18.3 1.2---11.8 2.3---9.9 1.4---16.5
Totalduration(s)
Mean 55.0±19.3 37.4±13.3 30.8±7.9 34.9±12.4 53.9±18.3 0.009
95%confidenceinterval 49.7---60.3 33.8---41.1 28.7---33.2 31.3---38.4 48.8---58.9
Min---max 24.4---133 14.7---73.4 18.2---54.9 18.2---73.5 17.3---97.7
DifferentstyletswiththeC-MACD-Blade 455
Time (sec)
125
100
75
50
25
0
NS
6
40 6
9
18 42
10 474
13
15
HS DS CS GEB
Figure 2 Total intubationtime according to group.NS, no stylet;HS, hockey-stickstylet;DS,D-bladetype stylet;GEB, gumelasticbougie;CS,CoPilotVLrigidstylet®.
complicationrates.Theuseofanappropriatestyleteased
passagepast thevocal cords andreduced thedurationof
intubation;intubationwasmorerapidlyaccomplishedusing
theDS,CSandHS,inthatorder.
Endotracheal intubation is among the most frequently
used life-saving interventions. Although technological
advanceshaveresultedinthedevelopmentofnoveldevices,
the classic Miller and Macintosh laryngoscopes remained
unequaled until the developmentof VL.Beginning in the
2000s,developmentsinVLtechnology,increasesinthe
avail-abilityofthesedevices,andthepositiveresultsshownby
scientific studieshave resulted in thesedevicesbecoming
considered the acme of airway management today. After
thedevelopmentofconventionalVLs, moreangledblades
that are suitable for use with difficult intubations were
developed.Whereas theconventional C-MAClaryngoscope
providesan18◦viewangle,theD-Bladeprovidesa40◦view
angle.Thisdifferenceinangleimprovestheoperator’sview
during laryngoscopy;however, inserting the tube into the
tracheaismoredifficult.8,15,16
Tocorrectlyadvancethetubethroughthetracheawith
aStorzC-MACD-Blade®VL,theuseofastyletisnecessary.
Changing the initial angle of the stylet or using different
typesofstyletsgreatlyfacilitatesintubation.Inthisstudy,
intubationdurationswereinvestigated.Durationsinvolving
thevisualizationofthevocalcords,cuffinflationandfirst
ventilationweresimilar;however,totalintubationduration
differedsignificantlybetweennotusingastyletandtheGEB
comparedtotheother intubationmethods (Table2).This
resultisapparentlyduetothepassageofthetubethrough
thetrachea.TheuseofanappropriatestyletwiththeStorz
C-MACD-Blade® easesthepassageofthetubethroughthe
tracheaandreducesthedurationofintubation,aswellas
increasesthepossibilityofsuccessfulintubationonthefirst attempt.Additionally,itwaspossibletocompletethe intu-bationwithoutadditionalmanipulation.Thisresultissimilar tothosefoundinpreviousstudies.11,17
HSareusedwithVLorwiththeclassicMacintosh
laryngo-scopefordifficultairwayinterventions.Astudycomparing
theuseofdifferentstyletswiththeStorzC-MAC®foundthat
thebestperformancewasobtainedusingthisstylettype.11
TheHSispreparedbyanglingthedistalendofthe
intuba-tiontubeata9---100◦angle.11,17However,usingthistypeof
styletcanmakestyletinsertionandremovalfromthe
intu-bationtubemoredifficult.Ithasbeenreportedthatdistal
tubeanglesofgreaterthan35◦canrenderpassagethrough
thetracheamoredifficult.18 Inourstudy,although intuba-tionwiththeHSprovidedbetterresultsthanuseofnostylet
orGEB,theresultsobtainedweresimilartothoseobtained
usinga rigid stylet with a smaller distal angle and those
obtainedusingaDS.
Rigidstyletscanalternativelybeusedtoeaseintubation
throughthetracheawhenperformingVL.Theirusepresents
noadvantagesovermalleablestyletswithdistalangles.19In ourstudy,theCo-PilotVL® rigidstyletwasused.Ina
liter-aturereview,wedidnotfindanypreviousstudyusingthis
stylet.Althoughintubationwasmorerapidusingthisstylet,
nodifferencesinintubationduration,successandtheneed
foradditionalmanipulationwerefoundwhencomparedto
theHS.Althoughbothstyletspresentadvantages,thestylet
preparedwiththebladeangle(DS)exhibitedequalsuccess
totheothertestedstylettypes.Althoughitappearsthatthe possibilityofdentaldamageusingthisstylettypeishigher,
webelievethatintubation withDSandD-BladeVLis
eas-ilyapplied.Importantly,thisstylettypepassedthetrachea mostquickly.Thisisprobablybecausetheangleofthetube isnotatthedistalend;thus,itadvancesmoreeasilyalong
theblade.
The portability, cheapness, availability, high success
ratesandeaseofuserendertheGEBanimportantlife-saving airwaydeviceforuseindifficultsituations.20Thismethodis
recommendedfordifficultairwayinterventionsbyDAS.The
resultsofmanystudiesundertakenworldwidehave shown
thattheGEBisthemostsuccessful,effectiveandcommonly
useddevice for use with a normal laryngoscope.21 In our
study,aGEBwasinsertedfirst;then,atube wasslidover
theGEBtoprovideintubation.Althoughthisrepresentsthe
classicuse,thisprocedure cancauseincreasedintubation
durationin practice.Various methods of using a GEB are
Table4 Complications.
Variable NS HS DS CS GEB p-Value
Dentaldamage 15(28.3%) 1(1.9%) 4(7.5%) 2(3.8%) 6(11.3%) <0.001
Useofexternallaryngealmanipulation,n(%)
BURPorOELM 53(100%) 7(13.2%) 6(11.3%) 7(13.2%) 31(58.5%) <0.001
NS,nostylet;HS,hockey-stickstylet;DS,D-bladetypestylet;GEB,gumelasticbougie;CS,CoPilotVLrigidstylet;BURP,cricoidpressure
available,suchasfirstinsertingtheGEBinthetubeor
insert-ingtheGEBsuchthatthetubeprotrudesfromtheMurphy
hole;thesemethodsarethoughttoaffectthedurationand
successofintubation.Intheirstudy,Batuwitageetal.did
notshowtheeffectsofdifferentusesofGEBonintubation
duration.Inthatstudy,similartoourown,theuseofGEB
didnotreducethedurationofintubation.17Inourstudyof
intubationduration,wefoundtheGEBdidnoteasepassage
throughthetrachea,andtheincreaseinthetotalintubation
durationwhenusingaGEBwasnotlinkedtothemethodof
GEBusebut wasduerathertodelaysininsertionintothe
trachea.UsingaGEBwiththeStorzC-MACD-Blade® VLdid
noteasepassagethroughthetrachea.
Limitations
Ourstudyuseda manikin; although conditionswere
stan-dardized,theinterventionsperformedmighthavediffered
fromreal-worldapplications.Inourstudy,onlydental
dam-agewasassessedasacomplication.Inclinicalapplications,
other complications, such asmucosal hemorrhage, larynx
damageandsubcutaneousemphysema,canoccur.The
appli-cations examined in this study might produce different
resultsinlivepatients.
Conclusion
Althoughobservation of the vocal cordsduring intubation
withthe Storz C-MAC D-Blade® VL,which is designed for
use with difficult airways, can be successful,it is
neces-sary to use an appropriate stylet for use with the blade
structureduring intubation.In ourstudy,intubationswith
nostyletandwithaGEBrequiredmoretimetocomplete,
requiredmoreattempts,andresultedinincreased
compli-cation rates.The D-Blade stylet,the rigidstylet, andthe
hockey-stickstylet(inthatorder)affordedmorerapid intu-bation,easierpassagepastthevocalcords,andreducedthe
durationofintubation.Becausethisstudyusedamanikin,
theresultsobtainedmight besimilartothoseobtainedin
humans in real-life situations; however, randomized
con-trolledhumanstudiesarewarrantedtoconfirmourresults.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
Acknowledgements
TheTrucorpAirSim® Advance Combomanikin usedinthe
studywasprovidedbytheTurkishdistributingfirmfor
tem-poraryuseinthestudy.Thisstudyhasnosponsor.
References
1.BurkleCM,WalshMT,HarrisonBA,etal.Airwaymanagement afterfailuretointubatebydirectlaryngoscopy:outcomesina largeteachinghospital.JAnaesth.2005;52:634---40.
2.KheterpalS,HealyD,AzizMF,etal.Incidence,predictors,and outcome ofdifficult maskventilationcombinedwithdifficult
laryngoscopy:areportfromthemulticenterperioperative out-comesgroup.Anesthesiology.2013;119:1360---9.
3.McKeenDM,GeorgeRB,O’ConnellCM,etal.Difficultandfailed intubation:incidentratesandmaternal,obstetrical,and anes-theticpredictors.CanJAnaesth.2011;58:514---24.
4.Budde AO, Desciak M, Reddy V, et al. The prediction of difficult intubation in obese patients using mirror indirect laryngoscopy: a prospective pilot study. J Anaesthesiol Clin Pharmacol.2013;29:183---6.
5.WallsRM,BrownCA3rd,BairAE,etal.Emergencyairway man-agement:amulti-centerreportof8937emergencydepartment intubations.JEmergMed.2011;41:347.
6.DieckT,KoppertW. HelsinkiDeclarationonPatientSafetyin Anaesthesiology---part9.Recommendationsforclinicalairway managementorganisation.AnasthesiolIntensivmedNotfallmed Schmerzther.2013;48:600---7.
7.ApfelbaumJL,HagbergCA,CaplanRA,etal.Practiceguidelines formanagementofthedifficultairway:anupdatedreportby theAmericanSocietyofAnesthesiologistsTaskForceon Manage-mentoftheDifficultAirway.Anesthesiology.2013;118:251---70. 8.CavusE, NeumannT, Doerges V, et al. Firstclinical evalua-tionoftheC-MACD-Bladevideolaryngoscopeduringroutineand difficultintubation.AnesthAnalg.2011;112:382---5.
9.XueFS, LiaoX,YuanYJ,etal.Rationaldesignofend-points toevaluateperformanceoftheC-MACD-Blade videolaryngo-scope during routine and difficult intubation. Anesth Analg. 2011;113:203.
10.Cavus E, Kieckhaefer J, Doerges V, et al. The C-MAC videolaryngoscope: first experiences with a new device for videolaryngoscopy-guided intubation. Anesth Analg. 2010;110:473---7.
11.McElwainJ,MalikMA,HarteBH,etal.Determinationofthe optimalstyletstrategyfortheC-MACvideolaryngoscope. Anaes-thesia.2010;65:369---78.
12.Behringer EC, Kristensen MS. Evidence for benefit vs nov-eltyinnewintubationequipment.Anaesthesia.2011;66Suppl. 2:57---64.
13.Al-Qasmi A, Al-AlawiW, MalikAM, etal. Assessmentof Tru-flexarticulatingstyletversus conventionalrigidPortex stylet asanintubationguidewiththeD-BladeofC-MAC videolaryngo-scopeduringelectivetrachealintubation:studyprotocolfora randomizedcontrolledtrial.Trials.2013;14:298.
14.GuptaAK,SharmaB,KumarA,etal.ImprovementinCormack andLehanegradingwithlaparoscopicassistanceduringtracheal intubation.IndianJAnaesth.2011;55:508---12.
15.Serocki G, Neumann T, ScharfE, et al. Indirect videolaryn-goscopywith C-MACD-Blade and GlideScope: a randomized, controlledcomparisoninpatientswithsuspecteddifficult air-ways.MinervaAnestesiol.2013;79:121---9.
16.JainD,DhankarM,WigJ,etal.Comparisonoftheconventional CMACandtheD-bladeCMACwiththedirectlaryngoscopesin simulatedcervicalspineinjury---amanikinstudy.BrazJ Anes-thesiol.2014;64:269---77.
17.Batuwitage B, McDonald A, Nishikawa K, et al. Comparison betweenbougiesandstyletsforsimulatedtrachealintubation withtheC-MACD-bladevideolaryngoscope.EurJAnaesthesiol. 2014:26.
18.LevitanRM,PisaturoJT,KinkleWC,etal.Styletbendangles andtrachealtubepassageusingastraight-to-cuffshape.Acad EmergMed.2006;13:1255---8.
19.JonesPM,LohFL,YoussefHN,etal.Arandomizedcomparison oftheGlideRite(®)Rigid Stylettoamalleablestyletfor
oro-trachealintubationbynovicesusingtheGlideScope(®).CanJ
Anaesth.2011;58:256---61.
20.JohnM,AhmadI.Preloadingbougiesduringvideolaryngoscopy. Anaesthesia.2015;70:111---2.