REVISTA
BRASILEIRA
DE
ANESTESIOLOGIA
PublicaçãoOficialdaSociedadeBrasileiradeAnestesiologiawww.sba.com.br
SCIENTIFIC
ARTICLE
Randomized
prospective
study
of
three
different
techniques
for
ultrasound-guided
axillary
brachial
plexus
block
Leonardo
Henirque
Cunha
Ferraro
∗,
Alexandre
Takeda,
Paulo
César
Castello
Branco
de
Sousa,
Fernanda
Moreira
Gomes
Mehlmann,
Jorge
Kiyoshi
Mitsunaga
Junior,
Luiz
Fernando
dos
Reis
Falcão
UniversidadeFederaldeSãoPaulo(UNIFESP),EscolaPaulistadeMedicina(EPM),DisciplinadeAnestesiologia,DoreMedicina Intensiva,SãoPaulo,SP,Brazil
Received26August2016;accepted17April2017 Availableonline16August2017
KEYWORDS
Axillarybrachial plexusblock; Ultrasound;
Perineuraltechnique; Perivascular
technique; Vascularpuncture
Abstract
Introduction:Randomizedprospectivestudycomparingtwoperivasculartechniqueswiththe perineuraltechniqueforultrasound-guidedaxillarybrachialplexusblock(US-ABPB).The pri-maryobjectivewastoverifyiftheseperivasculartechniquesarenoninferiortotheperineural technique.
Method: 240 patients were randomized to receive the techniques: below the artery (BA), aroundtheartery(AA)orperineural(PN).The anestheticvolumeusedwas40mLof0.375% bupivacaine.Allpatientsreceivedamusculocutaneousnerveblockadewith10mL.InBA tech-nique,30mLwereinjectedbelowtheaxillaryartery.InAAtechnique,7.5mLwereinjected at4 pointsaround the artery.In PN technique, themedian, ulnar, and radialnerves were anesthetizedwith10mLpernerve.
Results:Confidenceinterval analysis showed thattheperivascular techniquesstudied were notinferiortotheperineuraltechnique.Thetimetoperformtheblockadewasshorterforthe BAtechnique(300.4±78.4s,396.5±117.1s,487.6±172.6s,respectively).ThePNtechnique showedalowerlatencytime(PN---655.3±348.9s;BA---1044±389.5s;AA---932.9±314.5s), and less total time for the procedure (PN --- 1132±395.8s; BA --- 1346.2±413.4s; AA ---1329.5±344.4s).BAtechniquehadahigherincidenceofvascularpuncture(BA---22.5%;AA ---16.3%;PN---5%).
Conclusion:The perivascular techniquesareviable alternatives toperineuraltechnique for US-ABPB.ThereisahigherincidenceofvascularpunctureassociatedwiththeBAtechnique. ©2017PublishedbyElsevierEditoraLtda.onbehalfofSociedadeBrasileiradeAnestesiologia. Thisisanopenaccess articleundertheCCBY-NC-NDlicense(http://creativecommons.org/
licenses/by-nc-nd/4.0/).
∗Correspondingauthor.
E-mail:leohcferraro1@hotmail.com(L.H.Ferraro).
https://doi.org/10.1016/j.bjane.2017.07.001
PALAVRAS-CHAVE
Bloqueioplexo braquialviaaxilar; Ultrassom;
Técnicaperineural; Técnicaperivascular; Punc¸ãovascular
Estudoprospectivorandomizadodetrêsdiferentestécnicasparaobloqueiodoplexo braquialviaaxilarguiadoporultrassom
Resumo
Introduc¸ão: Estudoprospectivorandomizado,comparaduastécnicasperivascularescoma téc-nicaperineuralparaobloqueiodoplexobraquialviaaxilarguiadoporultrassom(BPVA-USG). Objetivo primário foi verificarse essastécnicas perivasculares sãonão inferioresà técnica perineural.
Método: Foramrandomizados240pacientesparareceberastécnicas:abaixodaartéria(TA),ao redordaartéria(TR)ouperineural(PN).Ovolumedeanestésicousadofoi40mldebupivacaína 0,375%. Em todosos pacientes, fez-se o bloqueiodo nervomusculocutâneo com 10ml. Na técnicaTA,injetaram-se30mlabaixodaartériaaxilar.NatécnicaTR,injetaram-se7,5mlem quatro pontosao redordaartéria. NatécnicaPN, osnervosmediano, ulnare radialforam anestesiadoscom10mlpornervo.
Resultados: Análisedosintervalosdeconfianc¸amostrouqueastécnicasperivasculares estu-dadas não são inferioresàtécnica perineural. A técnicaTA apresentou menor tempo para obloqueio(300,4±78,4seg;396,5±117,1 seg;487,6±172,6seg;respectivamente).A téc-nicaPNapresentou menortempodelatência(PN-655,3±348,9seg;TA-1044±389,5seg; TR -932,9±314,5 seg)e menortempo total deprocedimento(PN -1132±395,8 seg; TA -1346,2±413,4seg;TR1329,5±344,4seg).AtécnicaTAapresentoumaiorincidênciadepunc¸ão vascular(TA-22,5%,TR-16,3%;PN---5%).
Conclusão:Astécnicasperivascularessãoopc¸õesviáveisàtécnicaperineuralparaoBPVA-USG. Ressalta-semaiorincidênciadepunc¸ãovascularassociadaàtécnicaTA.
©2017PublicadoporElsevierEditoraLtda.emnomedeSociedadeBrasileiradeAnestesiologia. Este ´eum artigo Open Access sob umalicenc¸aCC BY-NC-ND(http://creativecommons.org/
licenses/by-nc-nd/4.0/).
Introduction
The ultrasound-guided technique for axillary brachial plexusblock(ABPB)ensurestheneedlecorrectplacement regarding the plexus, reduces the need for high volume and concentration of local anesthetic when it is injected around the nerves.1---3 With this ultrasound-guided
tech-nique,knownasperineuraltechnique,thelocalanesthetic isdeposited aroundthebrachialplexusterminal branches in the axilla. Although effective, this technique may be difficult toapplyby anesthesiologists intraining, particu-larlybecauseof thedifficulty in locatingthe radialnerve despite the use of ultrasound due to its position in rela-tiontothe artery.4Moreover,toapplythis technique,the
needleisrepositionedafewtimestoreachthenerve struc-tures,whichincreasesthechanceofparesthesiaduringthe procedure.
Theuseofultrasoundinregionalanesthesiahasprovided a redefinition for accomplishing some blockades, allow-ing theapplication of optional techniques toperform the sameblockade.Foraxillaryroute,inordertofacilitatethe blockadeanddecrease thenumberof timestheneedleis repositionedduringitsaccomplishment,ultrasound-guided techniqueswiththelocalanestheticapplicationonlyaround the axillary artery were described in the literature.5---7
Thesetechniqueswereapparentlyaseffectiveasthe per-ineural technique without altering the procedure time and decreased the incidence of paresthesia during the blockade.5---7However,theperivasculartechniqueincreased
theriskofinadvertentvascularpuncture.6,7
Thus,in ordertoreduce theblockadeprocedure dura-tion, without altering the time and success rate and ensuring patient safety, our group intended to compare two techniques of perivascular injection with the per-ineural technique for ABPB, all guided by ultrasound. Consequently, we tested the hypothesis that the perivas-culartechniquesarenotinferiortothestandardperineural technique regarding axillary brachial plexus block (BPVA) success.Blockadetime,latencytime,totalproceduretime, andvascular puncture incidencefor each techniquewere recorded.
Case
series
and
method
The study was approved by the Ethics Committee of our institutionunderthenumber296,974andregisteredin clin-icaltrials.govunderthecodeNCT02073383.
Inclusion criteria were age over 18 and below 65 years; provision of written informed consent; indication for brachialplexus block for candidates undergoing anes-thesia for elective hand surgery;ASA I or II, according to the American Society of Anesthesiology; and body mass index (BMI)<35kg.m−2. Exclusion criteria were cognitive
impairmentoractivepsychiatriccondition,infectionatthe puncturesite,coagulopathy,andhistoryofallergyto bupi-vacaine.
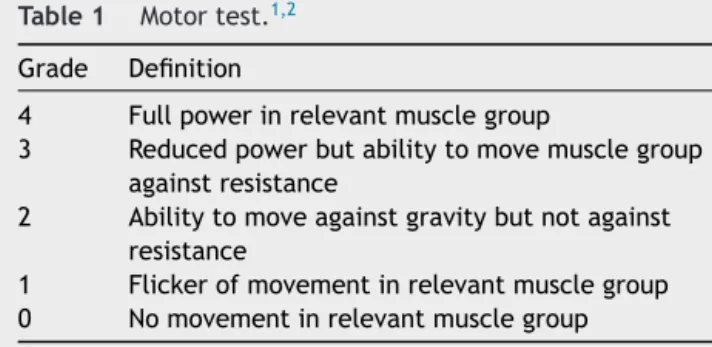
Table1 Motortest.1,2
Grade Definition
4 Fullpowerinrelevantmusclegroup
3 Reducedpowerbutabilitytomovemusclegroup againstresistance
2 Abilitytomoveagainstgravitybutnotagainst resistance
1 Flickerofmovementinrelevantmusclegroup 0 Nomovementinrelevantmusclegroup
pressure, and pulse oximetry. Intravenous access was obtainedinthecontralateralupperlimb.
Brachialplexusblockwasmadethroughtheaxillary path-wayusingultrasound(M-TurboRSystemwithHFL38×linear transducer 6---13MHz, SonoSite, Bothell, WA, USA), with thepatientplacedinthedorsalhorizontaldecubitus posi-tion. The needle used was 22G×50mm (AEQ2250, BMD Group,Venice,Italy).Afterasepsisandskinantisepsiswith chlorhexidine,analgesiaatthepuncturesitewasperformed with 1mL lidocaine 1%. Patients were divided into three groups:
Aroundtheartery technique(AA):30mLof 0.375% bupi-vacaine were injected aroundthe artery with 7.5mL of anestheticdepositedclockwiseatzero,3,6,and9-o’clock positions.
Below the artery technique (BA): 30mL of 0.375% bupi-vacaine wereinjected below thearteryat the 6-o’clock position.
Perineural technique (PN): 10mL of 0.375% bupivacaine wereinjectedaroundthemedian,ulnar,andradialnerves.
Additionally, the musculocutaneous nerve wasblocked with10mLof0.375%bupivacaineforallpatients.
Duringprocedure, the timerequired for theblockade, definedasthetimebetweenneedleinsertionandtheend oflocalanestheticinjection,wasrecorded.Blockadeswere performed byresidents andfellows of the institutionand supervisedbytwooftheauthors(L.H.C.F.andA.T.).
After local anesthetic injection, an observer who was not present during the procedure and who was blinded tothetechniqueevaluatedtheblockades. Thisevaluation wasdoneevery fiveminutes untilsurgical anesthesiawas obtainedorupto30minafterlocalanestheticinjection.The blockadelatencywasrecorded,definedasthetimebetween theendoflocalanestheticinjectionandthepatient achiev-ingasatisfactoryblockfortheprocedure.
Blockadeevaluation
Motorfunctionassessment
ThemodifiedBromagescalewasused(Table1).
The following muscles were evaluated: finger flexor (median nerve), finger extensor (radial nerve), thumb abductor (ulnar nerve), and elbow flexion (musculocuta-neousnerve).
Thermalsensitivityassessment
Theupperlimbthermalsensationevaluationwasperformed withgauzeandalcoholtotestthesensitivityofdermatomes innervated by the ulnar (hypothenar eminence), medial (volar regionofthe thumb),radial(dorsumofhand), and musculocutaneous (lateral region of the forearm) nerves. The cold sensation was considered as one and the non-perceptionofcoldaszero.
Painsensitivityassessment
The upper limb pain sensation evaluation wasperformed withthepinpricktestusinga23Gneedletotestsensitivity in regions of the ulnar, median, radial, and musculocuta-neousdermatomes.
Satisfactoryblockadewasdefinedaswithin30minutes thepatienthadmotorfunction≤2onthemodifiedBromage scale, absence of thermal sensitivity and of response to pinprickintheregionsofthemedian,ulnar,radial,and mus-culocutaneousnerves.Additionally,theprocedureshouldbe performedwithoutadditionalanalgesiatoconfirmthe anes-theticproceduresuccess.Thesatisfactoryblockaderateof eachgroupwasrecorded.
Subsequently,thetotalprocedure time,definedasthe sumofthetimerequiredfortheblockadepluslatencywas recorded.
Finally,theoccurrence ofaccidentalvascular puncture duringblockadewasrecorded.
Incaseofblockadefailure,patientsreceivedanesthetic supplementationattheelbowlevelwiththepreviouslyused solution.Afterblockadeassessment,patientswerereleased forsurgicalprocedureandreceivedmidazolam0.05mg.kg−1
forsedation.
Aftersurgicalprocedure,patientswereadmittedtothe post-anesthesiacareunit,wherethepostoperative analge-sia wasassessed usingthe visual analog scale, up tofour hoursaftertheblockadeintheunit.
Statisticalanalysis
TocalculatethesamplesizeneededtoshowthattheBAand AA techniques arenon-inferior toPN technique regarding surgerysuccessratethefollowingassumptionswere consid-ered.
Hypotheses
Null hypothesis. H0. pSAA−pSP≤−ı×optional
hypothe-sis:Ha:pSAA−pSP>−ı.
WithpSAAbeingtheproportionofsuccessexpectedinthe
BAtechniquesampleandpSP theexpectedsuccess ratein
thePNtechniquesample;ı=non-inferioritymargin.
Nullhypothesis. H0. pSRA---pSP≤−ı×hipóteseopcional:
Ha:pSRA−pSP>−ı.
WithpSRAbeingtheproportionofsuccessexpectedinthe
AAtechniquesampleandpSP theexpectedsuccess ratein
Non-inferiorityhypothesistest
1. Level of significance 1.25% (˛=0.0125 --- unilateral hypothesistestandtwoprimaryobjectives).
2. Samplepower80%(1−ˇ=0.80).
The expected proportion of success among the tech-niqueswasobtained throughtheanalysisof theliterature and apilot sample of the threetechniques performed by our group. Thus, a sample size of 240 patients (80 per group)reached apower of80%anda significancelevelof 1.25%(non-inferioritytestwithtwoprimaryobjectives)to showthatthebelowthearteryandaroundtheartery tech-niquesarenon-inferiortotheperineuraltechnique,witha non-inferioritymarginlowerthan12.5%.Thenon-inferiority hypothesis between groups was tested by comparing the lowerlimitofthe97.5%confidenceintervals.8
To compare the techniques regarding the quantitative variables (age, BMI, blockade time, latency, procedure time), the analysis of variance (ANOVA) was used with multiple comparisons of Bonferroni or, if necessary, the non-parametric Kruskal---Wallis test, followed by the non-parametricMann---Whitneytest.Forthequalitativevariable vascularpuncture,thechi-squaretestwasused.
Results
A total of 252 patients were included in the study,12 of whomwereexcludedduetoachangeinintraoperative surgi-caltechnique,withremovalofiliacbonegraftandtherefore conversiontogeneralanesthesiawasnecessary.Thegroups weresimilarregardingdemographicdataandpreoperative clinicalparameters(Table2).
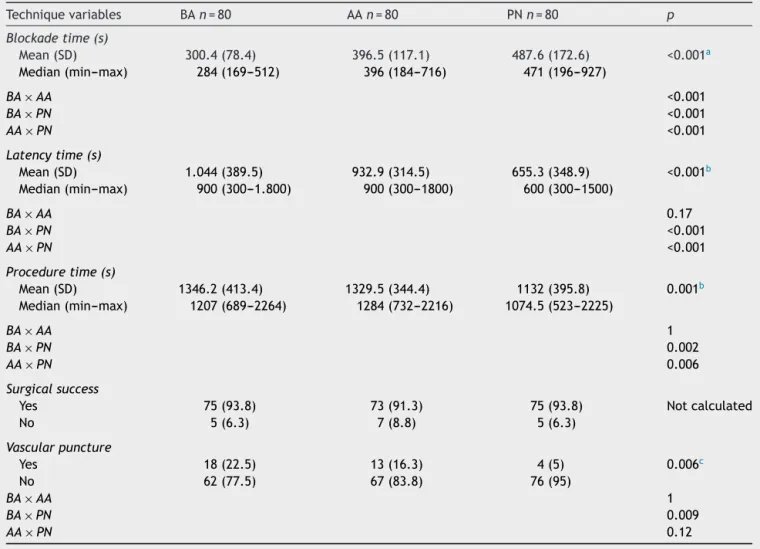
According to the results shown in Table 3 at the 5% significance level there was a significant difference between techniques regarding the following variables: timeinseconds(s)requiredforblockade,latency,procedure timeandvascularpuncture.
Regardingtheblockaderequiredtime,theBAtechnique showedamediantimesignificantlylowerthanthatforthe AAandPNtechniques.Inturn,thePNtechniqueshoweda blockademediantimesignificantlylongerthanthatforthe BAandAAtechniques(Table3).
Later,the PNtechnique showedamean latency signif-icantly lower than the average times for the BA and AA techniques,whichdidnotdiffersignificantlybetweenthem inmeanlatencytime(Table3).Furthermore,thePN tech-nique showed a mean procedure time significantly lower thanthatfortheBAandAAtechniques,whichalsodidnot differsignificantlyfromeach otherregardingmean proce-duretime(Table3).
Regarding vascular puncture,theBAtechnique showed apercentageofvascularpuncturesignificantlyhigherthan thatforthePN technique.However,AAtechniquedidnot differfromtheBAandPNtechniquesregardingthisvariable (Table3).
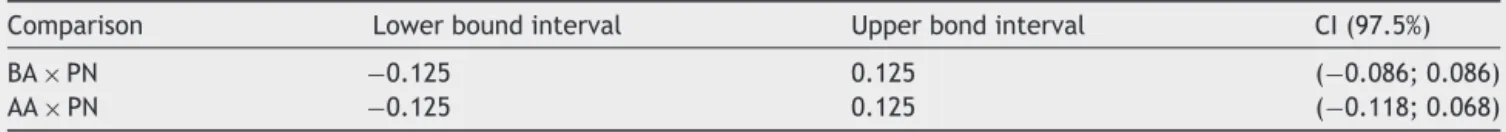
Regardingnon-inferiority,theresultsinTable4showthe lower limits of CI (97.5%) for the percentage difference betweensurgicalsuccessrates.Comparingthetechniques, theyarehigherthanthelowermarginofthenon-inferiority interval, not rejecting the hypothesis of non-inferiority betweentechniques(Table4).
Surgical procedures were uneventful. Regarding post-operative analgesia, no patient, whose blockade was considered satisfactory, referred pain up to 4h after the blockade. There was no complication, such as local anestheticintoxication,duringthestudy.Allpatientswere dischargedonthesamedayoftheprocedure.
Discussion
Inthis prospectiverandomized studyour group compared twoperivasculartechniqueswiththeperineuraltechnique forultrasound-guidedABPB.Wefoundthatthesingle injec-tionbelowthearteryand theinjectionaroundtheartery techniquesarenotinferiorcomparedtotheperineural tech-nique.
Imasogieetal. demonstratedthatthe localanesthetic injection near the artery provides a circumferential dis-persionaroundit (donutsign).5Apossible explanationfor
thisis thatthe tendency is forthe anesthetic todisperse toareasoflowerpressureinadjacenttissues.Thus,when thetechniqueisappliedbelowtheartery,thefascial pres-sureofthelatissimusdorsiposteriorlytothearterycauses theanesthetictodispersearoundtheartery andnotonly to the region below it.6 Other possible explanation is a
longitudinaldispersionofthelocalanestheticthroughthe neurovascular sheath of the axillary region.9 In order to
apply the perivascular techniques, the use of ultrasound isfundamental becauseitallowsvisualizingtheneedletip and local anesthetic dispersion during the blockade and ensuresthelocalanestheticcorrectdispersionaroundthe artery.Withoutusingultrasound,thesuccess rateof peri-vasculartechniquesislower,aslocalanestheticdispersion becomesunpredictable,needletipmaybetoodeep(within thelatissimus dorsifascia) or toosuperficial----outsidethe neurovascularsheath.9
Previous studies have suggested that the success rate amongperivasculartechniquesissimilartothatof perineu-raltechniqueforultrasound-guidedaxillarybrachialplexus block.Theratesrangedfrom87.5%to97.5%,similartothose foundin ourstudy.5---7,9 Moreover,studies haveshown that
perivasculartechniques wereperformed in ashorter time compared to perineural technique.5---7 However, in these
studies,asperineuraltechniquehadashorterlatency,the total blockade time that is the sum of blockade execu-tiontimepluslatencywassimilaramongthetechniques.5---7
Table2 Demographiccharacteristicsofpatients.
Techniquevariables BA AA PN Total p
Age(years)
Mean(SD) 40.8(13.6) 40.7(14.1) 38.4(12.4) 40(13.4) 0.433a
Median(min---max) 41.5(18---65) 39(19---67) 36(18---65) 39(18---67)
BMI(kg.m−2)
Mean(SD) 25.9(4.6) 26.7(3.8) 25.6(3.8) 26.1(4.1) 0.265a
Median(min---max) 25.6(14.7---39.1) 25.8(15.1---37.9) 25.2(16.8---34.5) 25.6(14.7---39.1)
ASA
I 35 36 37
II 45 44 43
Total 80 80 80
BA,belowtheartery;AA,aroundtheartery;PN,perineural;SD,standarddeviation.
aAnalysisofvariance(ANOVA).
Table3 Comparisonofblockadetechniquesaccordingtovariables:blockade,latencyandproceduretime,surgicalsuccess, andincidenceofvascularpuncture.
Techniquevariables BAn=80 AAn=80 PNn=80 p
Blockadetime(s)
Mean(SD) 300.4(78.4) 396.5(117.1) 487.6(172.6) <0.001a
Median(min---max) 284(169---512) 396(184---716) 471(196---927)
BA×AA <0.001
BA×PN <0.001
AA×PN <0.001
Latencytime(s)
Mean(SD) 1.044(389.5) 932.9(314.5) 655.3(348.9) <0.001b
Median(min---max) 900(300---1.800) 900(300---1800) 600(300---1500)
BA×AA 0.17
BA×PN <0.001
AA×PN <0.001
Proceduretime(s)
Mean(SD) 1346.2(413.4) 1329.5(344.4) 1132(395.8) 0.001b
Median(min---max) 1207(689---2264) 1284(732---2216) 1074.5(523---2225)
BA×AA 1
BA×PN 0.002
AA×PN 0.006
Surgicalsuccess
Yes 75(93.8) 73(91.3) 75(93.8) Notcalculated
No 5(6.3) 7(8.8) 5(6.3)
Vascularpuncture
Yes 18(22.5) 13(16.3) 4(5) 0.006c
No 62(77.5) 67(83.8) 76(95)
BA×AA 1
BA×PN 0.009
AA×PN 0.12
BA,belowtheartery;AA,aroundtheartery;PN,perineural;SD,standarddeviation.
aKruskal---Wallistest.
Table4 Non-inferiorityanalysisofthesurgicalsuccessrateoftheBAversusPNandAAversusPNtechniques.
Comparison Lowerboundinterval Upperbondinterval CI(97.5%)
BA×PN −0.125 0.125 (−0.086;0.086)
AA×PN −0.125 0.125 (−0.118;0.068)
BA,belowtheartery;AA,aroundtheartery;PN,perineural.
Onelimitationofourstudywasnotrecordingthe num-berofneedlerepositioningattempts duringblockades and theincidenceofparesthesiafoundineachtechnique. How-ever, this subject has already been well documented in previous studies showing that perivascular techniques are applied with less needle repositioning and lower rate of paresthesia.6,7
Thus, as perivascular techniques have a shorter exe-cutiontime,comparable totalprocedure time,and lower incidence of paresthesia, they are recommended for ultrasound-guided ABPB. So a protocol of two injections wasrecommended:oneinjectionintothemusculocutaneous nerveandoneinjectionbelowtheartery.7Furthermore,it
isbelievedthatthistechniqueismoreappropriatefor peo-plewithlessexperienceitmaybethetechniqueofchoice fortrainingthisblock.
However,afactconcerningthesafetyprocedureofthe BAtechniqueshouldbementioned.Oneofthegreat advan-tagesbroughtbytheultrasound-guidedregionalanesthesia technique,comparedtoothertechniquesforlocatingnerve structures, wasthe reduced number of accidental vascu-lar puncture, which is oneof the most important factors related to local anesthetic systemic intoxication.10 Thus,
ultrasoundwasabletoreducetheincidenceoflocal anes-thetic intoxicationcomparedto the neurostimulation and paresthesiatechniques.10However,studiesusingtheBA
sin-gleinjectiontechniqueforultrasound-guidedABPBshowed arelativelyhighincidenceofaccidentalvascularpuncture, rates well above that of perineural technique. Vascular puncture rates for BA and PN techniques were, respec-tively:Bernuccietal.(24%×0%);Choetal.(7%×0%);and Tran et al. (15%) for BA technique.6,7,9 Our results show
anincidenceofvascularpuncturesimilartoprevious stud-ies:22.5% for BAtechnique; 16.3% for AAtechnique, and 5%forperineuraltechnique.Vascularanatomicalvariations in axillary region are common and may complicate the axillary brachialplexus block.Kutiyanawalaetal. demon-stratedthat21of100patientsundergoingaxillarydissection had anatomical variations in this region, 10 of them had twoaxillary veins.11 Arteryvariations arealsocommonin
this region.12 This shows that, despite the other benefits
demonstratedbytheBAtechnique,suchasreducedneedle repositioningandlowerincidenceofparesthesia,it signifi-cantlyincreasesthechanceofaccidentalvascularpuncture and,perhaps,itshouldnotbethetechniqueofchoicefor patientswithcoagulationdisordersor vascularanatomical variations. Moreover, as in the single injection BA tech-nique,alargeamountoflocalanestheticisdeposited13and
frequent aspirations are suggested toincrease the safety of not applying an intravascular injection. Futurestudies shouldtrytocomparewhetherthisincreasedincidenceof
vascularpuncturemayincreasetheriskoflocalanesthetic systemictoxicitywiththeuse ofthistechnique.However, nohematomaorsignofsystemicintoxicationbylocal anes-theticwasrecordedinthepresentstudy.
Finally,itshouldberecognizedthattheperineural tech-nique allows the use of smaller volumes compared to perivasculartechniques,whichdecreasesthetotalmassof anestheticusedandensuresagreatermarginofsafety com-paredtothetoxicdoseoflocalanesthetic.1,2,13
Inconclusion,thepresentstudyshowedthatthe perivas-culartechniquesstudiedarenotinferiortotheperineural technique,whichmakesthemviableoptionsfor ultrasound-guidedaxillarybrachialplexusblock.However,careshould betakenregardingtheincreasedincidenceofvascular punc-ture when using these techniques, particularly the single puncturebelowthearterytechnique.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.O’DonnellBD,IohomG.Anestimationoftheminimumeffective anestheticvolumeof2%lidocaineinultrasound-guidedaxillary brachialplexusblock.Anesthesiology.2009;111:25---9.
2.FerraroLHC,TakedaA,RezendeAH,etal.Determinationofthe minimumeffectivevolumeofbupivacaine0.5%for ultrasound-guided axillary brachial plexus block. Rev Bras Anestesiol. 2014;64:49---53.
3.TakedaA, FerraroLH,RezendeAH,et al.Minimumeffective concentrationofbupivacaineforaxillarybrachialplexusblock guidedbyultrasound.RevBrasAnestesiol.2015;65:163---9.
4.WongDM,GledhillS,ThomasR,etal.Sonographiclocationof theradial nerveconfirmed bynervestimulation during axil-larybrachialplexusblockade.RegAnesthPainMed.2009;34: 503---7.
5.ImasogieN,Ganapathy S,SinghS, etal.A prospective, ran-domized,double-blindcomparisonofultrasound-guidedaxillary brachialplexusblocksusing2versus4injections.AnesthAnalg. 2010;110:1222---6.
6.Bernucci F,Gonzalez AP,Finlayson RJ, et al. A prospective, randomizedcomparison betweenperivascular and perineural ultrasound-guided axillarybrachial plexus block. Reg Anesth PainMed.2012;37:473---7.
7.ChoS,KimYJ,BaikHJ,etal.Comparisonofultrasound-guided axillarybrachialplexusblocktechniques:perineuralinjection versussingleordoubleperivascularinfiltration.YonseiMedJ. 2015;56:838---44.
9.TranDQ,PhamK,DuganiS,etal.Aprospective,randomized comparisonbetweendouble-,triple-,andquadruple-injection ultrasound-guided axillarybrachial plexus block. Reg Anesth PainMed.2012;37:248---53.
10.Neal JM.Ultrasound-guided regional anesthesia and patient safety:updateofanevidence-basedanalysis.RegAnesthPain Med.2016;41:195---204.
11.KutiyanawalaMA,StotterA,WindleR.Anatomicalvariants dur-ingaxillarydissection.BrJSurg.1998;85:393---4.
12.OrebaughSL,WilliamsBA.Brachialplexusanatomy:normaland variant.SciWorldJ.2009;9:300---12.